Background: CPX-351 has recently been approved for the treatment of patients diagnosed with Acute Myeloid Leukemia (AML) arising from a previous myelodisplastic syndrome (s-AML) or secondary to chemotherapy (t-AML) as per former WHO 2016 classification.
Minimal residual disease (MRD) assessment is a strong prognostic factor for relapse and shorter survival in AML patients undergoing intensive induction chemotherapy.
Recent studies explored the role of genomic profile of AML influencing clinical outcome. In particular, Papaemmanuil et al showed that mutations in critical genes such as TP53, ASXL1, SRSF2 and RUNX1 are independently associated with a worse prognosis; moreover, co-occurrence of different high-risk mutations are predictors of dismal outcome when conventional chemotherapy is administered.
Adverse risk mutations are particularly frequent in s-AML and t-AML. As clinical trials evaluating the prognostic relevance of MRD in the context of different molecular subsets mainly involve younger patients affected by de novo AML and receiving conventional 3+7 chemotherapy, there is a lack of data to define the impact of specific mutations on MRD clearance and prognosis in elderly s- AML and t-AML patients receiving CPX-351 induction.
Aims: The aim of this study was to evaluate the prognostic impact of recurrent genic mutations and mutational burden at diagnosis on CR probability, MRD clearance and prognosis in a cohort of elderly s-AML or t-AML patients treated with CPX-351 induction chemotherapy.
Methods: The study included 67 elderly patients (>60 year, median age 69, range 60-77) with a diagnosis of s-AML or t-AML according to WHO2016 classification, treated in our Center with CPX-351.
Next generation sequencing (NGS) was performed using the Myeloid Solution panel by SOPHiA Genetics, encompassing 34 critical genes mutations. Sample have been processed on a Illumina MiSeq platform and the analysis performed with SOPHiA DDM® Software. MRD was analysed in all patients achieving complete remission (CR) with multicolour flow-cytometry, with a threshold of 0.1%.
Results: AML patients were re-classified according to ELN 2022 risk score which was adverse, intermediate and favourable in 35, 29 and 3 patients, respectively. Median number of mutations for single patient (mutational burden) by NGS was 4 (range 2-9). Most frequent mutations involved: RUNX1 (44%), ASXL1 (37%), TP53 (33%), IDH1 (18%), IDH2 (14%), DNMT3A (14%), TET2 (8%).
Four patients died before response assessment, mainly due to infections.
Fifty-four patients (81%) achieved complete remission (CR) after first induction cycle; MRD evaluation was negative in 28/54 responding patients (52%).
Univariate and multivariate analysis showed that factors traditionally associated with poor outcome such as ELN risk group, leukocytosis at diagnosis or previous treatment with hypomethylating agents did not affect the probability of CR rate and MRD negativity. Interestingly, having any high risk mutation, the combination of ≥2 high risk mutations or high mutational burden (having ≥ 4) did not affect CR probability and MRD negativity rate both in univariate and multivariate analysis.
After cycle 2, the cumulative CR rate was 56/67 (84%), with 33/56 (59%) responding patients obtaining MFC MRD negativity.
After a median follow up of 36 months (CI 95%; 22.4 -48.5 months), median OS was 19 months (CI 95% 13-24), whereas 2 year OS was 24%.
Multivariate OS analysis revealed that negative MRD was the strongest independent predictor of longer survival (p<0.05).
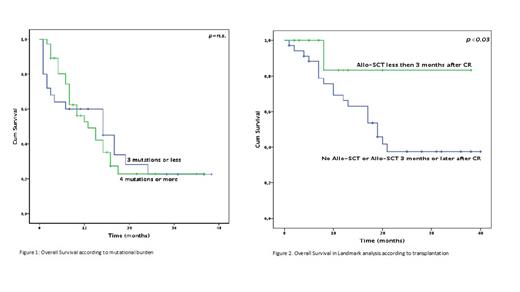
Notably, OS was not affected by mutational burden (29.2% and 27.6% for patients with less or more than 4 mutations, respectively, p=n.s, Fig.1).
In landmark analysis, patients achieving CR and proceeding to allogeneic stem cell transplantation consolidation (HSCT) within 3 months from CR (N=13) had a significantly better outcome if compared to CR patients who did not receive HSCT or proceeded to transplant later (N= 41, 2-year OS: 84.6% and 31.7, respectively, p<0.03, Fig. 2).
Conclusion : CPX-351 is able to induce good quality remission with high CR rate and MRD negativity, regardless of mutational burden, allowing a high number of elderly AML patients to undergo to HSCT. MRD evaluation has proven to be a strong prognostic tool also in the setting of elderly s-AML and t-AML patients receiving CPX-351. The prognostic value of high risk mutation seems to be less relevant in CPX-351 treated patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal